News
July 26, 2024
Highlights from ACOG: New guidelines for omega-3 DHA + EPA supplementation and intake to reduce risk of preterm birth
Explore new clinical guidelines for higher dose omega-3, DHA and EPA, for pregnant women to help reduce the risk of preterm birth, presented by the leading authors at the recent ACOG meeting.

Summary
- With preterm birth rates increasing in some countries, there is an urgent need to better support women before and during pregnancy so they can deliver healthy, full-term babies.1
- At the recent American College of Obstetricians and Gynecologists (ACOG) Annual Meeting, dsm-firmenich hosted a session spotlighting new global clinical practice guidelines for omega-3 fatty acid intakes before and during pregnancy to reduce preterm birth risk, presented by the lead authors of the guidelines.
- Read on to explore the compelling data behind the role of the omega-3 docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) in reducing the risk of preterm births, especially for high-risk groups, as well as specific omega-3 intake recommendations for before and during pregnancy.
Every year, an estimated 13 million babies worldwide are born preterm (before 37 weeks), and rates are rising in many countries like the United States (US).1,2 In the US, preterm birth is a leading cause of infant mortality, with a staggering one in ten babies born preterm.3 Moreover, the burden disproportionately impacts certain racial and ethnic groups. Non-Hispanic Black women face a 55% higher risk of preterm birth and a 115% higher risk of early preterm birth (before 34 weeks) compared to White women.4 Recent studies have shown that women with low omega-3 or DHA intakes early in pregnancy have an increased risk of preterm and early preterm birth.5,6 The financial impact of preterm birth is staggering, with estimates revealing that it cost the US $34.5 billion in healthcare costs in 2021, with almost $23 billion of that attributed to early preterm birth.7
Improving full-term birth rates to reduce the risk of infant mortality and disability is a global health priority. Fortunately, new clinical practice guidelines highlight a promising, science-backed solution to reduce the risk of preterm birth – adequate intakes of the omega-3 fatty acids DHA and EPA for women before and during pregnancy.8 Read on to explore the latest scientific evidence behind this prenatal nutrition intervention and expert recommendations for omega-3 intakes and supplements across the motherhood journey.
New omega-3 guidelines spotlighted at ACOG
Tackling the prevalence of preterm birth was a focus at this year’s ACOG Annual Clinical and Scientific Meeting in San Francisco, California, on May 17-19. With over 60,000 members, ACOG is the leading group of physicians providing obstetric and gynecologic care in the US. We had the pleasure of attending the annual meeting along with other industry experts, healthcare practitioners, scientists and patient educators. Our mission? As part of dsm-firmenich’s larger Every Day Counts campaign, we aimed to raise awareness of the new clinical practice guidelines recommending higher doses of omega-3/DHA and EPA supplements, especially for women with low baseline intakes as a solution to reduce preterm birth risk. To connect with as many delegates as possible, we participated in not one, but two booths at the meeting – one of which was hosted in collaboration with the Council for Responsible Nutrition (CRN) and five other industry partners. The CRN booth was designed as a Prenatal Nutrition Center, highlighting that over 90% of pregnant women are not meeting their nutrient needs from diet alone.9
The evidence for high dose DHA supplements
On the final day of the meeting, we hosted a Product Theatre Session spotlighting the new clinical practice guidelines for DHA (or DHA and EPA) supplementation to help reduce the risk of preterm birth, published in a leading obstetrics journal, American Journal of Obstetrics & Gynecology Maternal-Fetal Medicine (AJOC MFM), in February 2024.8 The session was moderated by Dr. Emily DeFranco (John W. Greene Endowed Professor and Chair Department of Obstetrics & Gynecology at the University of Kentucky) and the guidelines were shared by the primary authors, Dr. Susan Carlson (AJ Rice Professor of Nutrition and University Distinguished Professor, University of Kansas Medical Center) and Dr. Irene Cetin (Professor of Obstetrics and Gynecology, University of Milan Head of Obstetrics Unit, Mangiagalli). Dr. Carlson opened by highlighting that pregnant women in the US have very low intakes of fish, which is the main dietary source of omega-3 fatty acids including DHA.10
Next, Dr. Carlson presented key findings from a 2018 Cochrane Review, which found high quality evidence that omega-3 supplementation during pregnancy could reduce the risk of preterm birth by 11% and early preterm birth by 42%.11 Critically, Dr. Carlson shared findings from her ADORE study that compared the impact of providing 200mg vs 1,000mg of algal DHA daily in pregnant women on the risk or preterm and early preterm births. Overall, the results of the analysis demonstrated that the 1,000mg dose was superior to the 200mg dose and significantly reduced preterm birth by 25%. The higher dose also resulted in a 29% reduction in early preterm birth, although it was not quite statistically significant.5 However, for women who entered the clinical trial with low baseline DHA status, the higher dose reduced early preterm birth by an impressive 48%.5
Moreover, her study showed that adequate intake is important even before pregnancy. Women who entered pregnancy with adequate DHA intakes (as reflected by higher blood DHA levels) were already at a substantially reduced risk of both preterm and early preterm birth. Even in mothers with high DHA blood status, further supplementation significantly reduced preterm birth, demonstrating that these mothers still need continued DHA throughout pregnancy. For mothers with low baseline DHA status, supplementing with 1,000mg DHA reduced preterm births by 26% and early preterm births by a striking 48% compared to the lower, 200mg DHA dose.5 Dr. Carlson also shared results from her study suggesting that Black women benefited most from having both an adequate baseline DHA intake and a higher dose (1,000mg) DHA supplementation.12 This data reinforces that high dose DHA, especially for women with low baseline DHA intakes, can significantly improve the chances of having a full-term birth.
Next, Dr. Carlson addressed a burning question – how can we identify women who are at risk of preterm birth due to low omega-3 levels, and would therefore benefit from higher dose supplementation? She explained that a validated food frequency questionnaire can estimate a woman’s DHA intake levels during early pregnancy based on consumption of fish, egg yolk, chicken, liver and supplements containing DHA.13 This survey provides healthcare practitioners with a tool to assess patient DHA status and make appropriate supplement recommendations.
What do the new clinical DHA guidelines recommend?
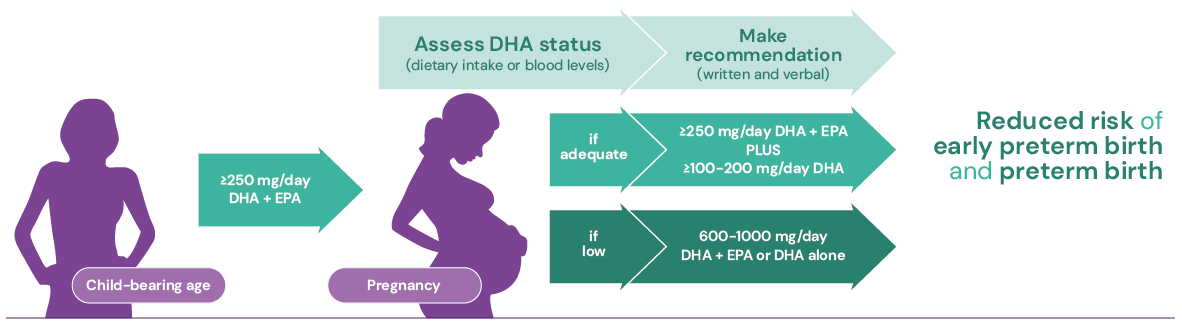
In the second half of the session, Dr. Irene Cetin presented key recommendations from the newly published guidelines for omega-3 intakes and supplementation before and during pregnancy:8
- Preconception stage: Getting adequate DHA intake during preconception is crucial, as women with low DHA levels or intake early in pregnancy face an increased risk of preterm birth. The guidelines advise all women of childbearing age to ensure a regular omega-3 intake of at least 250mg per day of DHA alone or in combination with EPA.
- During pregnancy: Throughout pregnancy it is recommended that all women consume an extra 100-200mg of DHA daily, totaling at least 350-450mg of DHA alone or EPA and DHA combined.
- High-risk pregnancies: Women identified as having low omega-3 or DHA intake/status early in pregnancy face a higher risk of both preterm and early preterm birth. To address this elevated risk, the guidelines advise supplementing with higher daily doses of 600-1,000mg of DHA alone or in combination with EPA.14
By following these tailored recommendations at each stage, pregnant women can ensure they reach the omega-3 levels shown to reduce the risk of preterm birth.
The potential for massive impact
The potential impact of tailored omega-3 recommendations for every woman of childbearing age could be transformative. If all pregnant women were able to supplement with an effective DHA dose, experts estimate it could help prevent over 40,000 preterm births each year in the US alone.7 What’s more, DHA no longer needs to come at a cost to marine ecosystems, as algal-oil omega-3s – such as our life’s®OMEGA – offer a more sustainable, more potent and more enjoyable to consume alternative to fish oil. Research from Frost & Sullivan estimates that supplementing all pregnant women with protective levels of algal DHA could save the US over $8 billion each year.7 With such significant benefits for mothers, babies and healthcare costs, increasing access to adequate doses of high quality DHA supplementation must be a public health priority.9
Unlock the benefits of omega-3s for a healthy pregnancy
Discover more about how omega-3s play a crucial role in building the foundation for a health pregnancy.
References
1 World Health Organization, Preterm birth. Key facts. Available at: https://www.who.int/news-room/fact-sheets/detail/preterm-birth
2 Martin JA, et al. (2023) Births in the United States, 2022. NCHS Data Brief, no 477. National Center for Health Statistics.
3 152 million babies born preterm in the last decade. Pan American Health Organization, Jun 2023
4 Hamilton BE, et al. (2023) Births: Provisional Data for 2022. NVSS Vital Statistics Rapid Release, Report No. 28.
5 Carlson et al., Higher dose docosahexaenoic acid supplementation during pregnancy and early preterm birth: A randomized, double-blind, adaptive-design superiority trial. EClinMed 36 (2021) 100905.
6 Simmonds et al, (2020). Omega-3 fatty acid supplementation in pregnancy-baseline omega-3 status and early preterm birth: exploratory analysis of a randomised controlled trial. BJOG : an international journal of obstetrics and gynaecology, 127(8), 975–981.
7 Frost & Sullivan. Reducing the economic impact of preterm and early preterm birth in the United States by providing supplemental algal DHA to expectant mothers. Available at: Health Economics | Every Day Counts
8 Cetin, I. et al. (2024) Clinical Practice Guideline on behalf of Asia Pacific Health Association (Pediatric-Neonatology Branch), Child Health Foundation (Stiftung Kindergesundheit), European Academy of Paediatrics, European Board & College of Obstetrics and Gynaecology, European Foundation for the Care of Newborn Infants, European Society for Paediatric Research, and International Society for Developmental Origins of Health and Disease. Omega-3 fatty acid supply in pregnancy for risk reduction of preterm and early preterm birth. American journal of obstetrics & gynecology MFM, 6(2), 101251.
9 Regan L. Bailey, PhD, MPH, RD; Susan G. Pac, MS, RD; Victor L. Fulgoni III, PhD; Kathleen C. Reidy, DrPH, RD; Patrick M. Catalano, MD. Estimation of Total Usual Dietary Intakes of Pregnant Women in the United State. JAMA Network Open. 2019;2(6).
10 Zhang Z, Fulgoni VL, Kris-Etherton PM, Mitmesser SH. Dietary Intakes of EPA and DHA Omega-3 Fatty Acids among US Childbearing-Age and Pregnant Women: An Analysis of NHANES 2001-2014. Nutrients. 2018;10(4):416. Published 2018 Mar 28.
11 Middleton et al., Omega-3 fatty acid supplementation during pregnancy, Cochrane Review 2018.
12 DeFranco EA, Valentine CJ, Carlson SE, Sands SA, Gajewski BJ. Racial disparity in efficacy of docosahexaenoic acid supplementation for prevention of preterm birth: secondary analysis from a randomized, double-blind trial. Am J Obstet Gynecol MFM. 2024;6(5):101358. doi:10.1016/j.ajogmf.2024.101358
13 Christifano DN, Crawford SA, Lee G, Gajewski BJ, Carlson SE. (2022) Utility of a 7- question online screener for DHA intake. Prostaglandins Leukot Essent Fatty Acids;177:102399.
14 Cetin I, Carlson SE, Burden C, et al. Omega-3 fatty acid supply in pregnancy for risk reduction of preterm and early preterm birth. Am J Obstet Gynecol MFM 2024;6:101251.
Related Content
Recommended Reading
-

17 June 2024
Pharma’s next frontier: Explore 4 trends shaping the future of the pharmaceutical industry
-

2 April 2024
New study spotlights necessity for preconception guidance to fill potential nutrient gaps
-

17 November 2023
World Prematurity Day: DHA supplementation to reduce preterm birth risk for pregnant women
Quick links
Customized blends of functional ingredients in one single, efficient premix.
Streamline your product development process and get to market faster.
Solutions to address consumers' health and lifestyle needs, giving you an edge in the market.
Talking Nutrition, Health & Care
Explore new science, consumer insights, industry news and more in our latest articles.
Discover educational whitepapers, webinars, publications and technical information.
Request samples, place orders and view product documentation.